Streptococci in a smear in women: should I worry and is it dangerous? What to do if streptococcus is detected in a smear
is a pathogenic microorganism that leads to disorders in many organs and systems of the body. Penetrating the mucous membranes, it rapidly affects the nasopharynx, intestines, genitourinary tract and respiratory system.
The bacterium is capable of localizing in one or several organs at the same time. This requires immediate diagnosis and therapeutic intervention.
If found, this means that a pathogenic bacterium has entered the human body. What is it, how is it dangerous and how does it get into organs and systems?
Streptococcus is a pathogenic microorganism that is found in the microflora of any person. He is its normal complement. However, under the influence of provoking factors, the microbe is reborn and begins to “attack” the organs and systems of its own body.
Streptococcus
In most cases, sedimentation of bacteria is recorded in the nasopharynx, respiratory tract, genitourinary system and intestines. The development of streptococcal infection occurs with a sharp weakening of protective functions body.
Rapid penetration into organs and systems can provoke a negative reaction large quantity unknown strain of pathogens.
It should be noted that not all microbes are dangerous to health. Some representatives are beneficial. Do not perceive the presence of microbes in the body as something scary.
In microflora healthy person there are always bacteria. This is a universal defense of the body, thanks to which the immune system fights many diseases.
All streptococci :
- non-hemolytic.
The most significant representatives are beta-hemolytic streptococci. They are considered to be the causative agents of many diseases in the human body. Under their influence, sore throat, laryngitis, pharyngitis and pneumonia develop. Streptococcus agalactiae in a smear indicates inflammatory processes in the genitourinary system.
How does bacteria enter the human body? There are many ways of transmission, the most common are: contact, sexual, airborne and food. Failure to comply with hygiene rules, consumption of dirty products, insufficient processing of meat and fish, contact with a sick person - all this leads to infection.
Compliance elementary rules hygiene and attention to one’s own health will help prevent the development of dangerous diseases.
How to detect the presence of streptococcus
How to take a smear for streptococcus and? The study is carried out in conditions medical institution. To do this, you need to seek help from your local therapist. Based on the patient’s complaints and examination, he will issue a referral for further procedures.
Express test
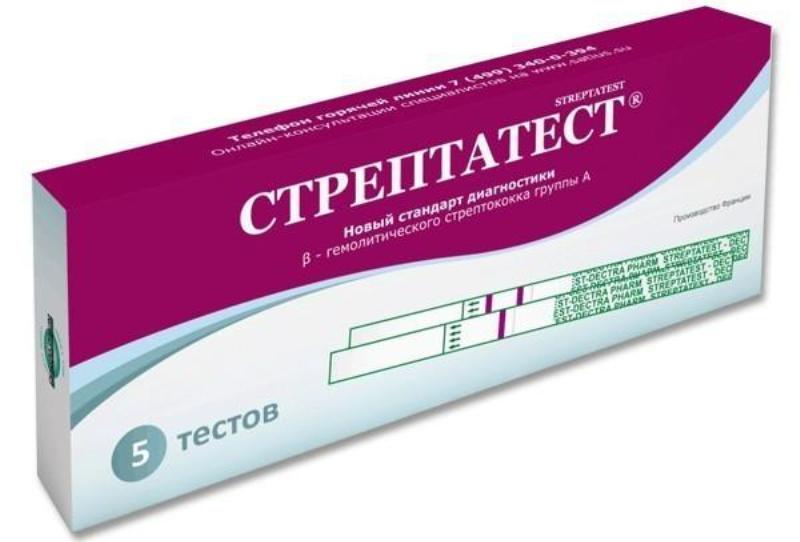
Streptatest rapid test for determining streptococcus
Today there are both quick tests, and long-term laboratory studies. The first type of determination of bacteria in the body is a rapid test. It is carried out both in a hospital and at home.
To carry it out, you need to purchase a special test. The standard kit includes a special flask, 2 bottles of liquids, cotton swab and express strip.
A person needs to take a swab (throat, tonsils, genitals) themselves. Before this, a special flask is prepared, into which 4 drops are first poured from a red bottle, then from a yellow one.
A cotton swab (smear) is rolled in the resulting mixture 10 times and then left for one minute. Next, it is removed and an express strip is sent into the resulting “microbial” liquid.
Within 5 minutes the result will be ready. One strip means the test is negative, two strips mean the test is positive. In total, it takes about 30 minutes to determine the result.
If streptococcus is detected in the smear, it is necessary to consult a doctor regarding further treatment tactics.
Laboratory research
Streptococcus epidermis in a smear is also determined through a routine laboratory test. The result is known no earlier than after 2-5 days. The purpose of the study is to determine the pathogen, its identification and determination of sensitivity to antibiotics.
A smear is taken from a man's urethra or a woman's vagina. Determining the presence of cocs in a normal environment is not difficult. It is much more difficult to identify their type.
Before taking a smear, a person must prepare thoroughly. It is not recommended to carry out hygiene procedures on the eve of the study. It is not advisable to go to the toilet 2-3 hours before taking the material.
Any drug therapy eliminated within 24-48 hours. Taking medications can affect the reliability of the results. It is also necessary to abstain from sexual intercourse for 2-3 days.

A smear for streptococcus is taken from the urethra of a man or the vagina of a woman
After taking the material, its examination is carried out for 2-5 days. During this process, special reagents are used. If the study reveals streptococcus in a smear in men or women, a consultation is held.
What to do if streptococci are detected
The causes of streptococcus in a smear in women and men are often associated with promiscuity, unprotected intercourse and weak immunity. All this is closely interconnected. To become infected, it is enough to have contact with a sick person.
Streptococci in men
If streptococcus is detected in a man's smear, mandatoryit is necessary to consult a specialist. The presence of bacteria requires immediate medicinal treatment.
Elimination pathological processes in organs genitourinary system carried out using two groups of drugs: antibiotics and non-steroidal anti-inflammatory drugs (NSAIDs).
Antibiotics stop the activity of potentially dangerous microbes, and NSAIDs fight the inflammatory process.
Antibiotics are selected on an individual basis. In most cases, Azithromycin, Tsiprolet and Kanamycin are used. Their effectiveness is tested by a specialist in laboratory conditions.
Streptococci are not susceptible to the influence of all antibiotics; this fact must be taken into account. Exposure to bacteria for 5-7 days allows you to completely eliminate them from the body.
Therapy is supplemented with non-steroidal anti-inflammatory drugs (Diclofenac, Indomethacin).
Streptococci in women

Ampicillin
Symptoms of streptococcus in a smear in women depend on the individual characteristics of the organism. In most cases, discharge is recorded, bad smell, itching and burning during urination. Is not specific symptoms. They may indicate a number of other diseases.
The presence of bacteria can only be determined laboratory test. The reasons for their appearance in a woman’s body are similar to those in men.
Staphylococci and streptococci in a smear in women indicate acute inflammatory processes in the genitourinary system. If pathogenic microorganisms were identified during the study, it is necessary to proceed additional research. After a full range of diagnostic measures, complex therapy is prescribed.
Treatment of streptococcus in a smear in women involves the use of antibiotics. The most effective are drugs belonging to the penicillin series. Antibiotics are selected on an individual basis. In most cases they use Ampicillin And Benzylpenicillin. For elimination local manifestations inflammatory process, apply Betadine cream.
Streptococci are pathogenic microorganisms that are found in the body of every person. There is no specific vaccine against them. The presence of streptococci in a smear may be within normal limits or beyond acceptable levels. In this case, the person is prescribed complex treatment.
In contact with
Streptococcus in a smear
Streptococcal infection may be in various areas human body. Most often it lives in the digestive system, oral cavity, nose, and also in the female genital organs. If you are diagnosed with streptococcus in a smear, do not be alarmed, as this family of microorganisms can be successfully treated in our time. But one should not be indifferent to this either. Streptococcal infection, if not treated, can cause a number of serious illnesses. There are several types of streptococcus pathogens. It follows from this that, having detected coca in a smear, treatment is prescribed by gynecologists, urologists, pulmonologists and other specialists, depending on in which organs the infection is localized. When prescribing therapy, age and individual characteristics the sick body.
Routes of infection
Penetration of streptococcus into the body of a healthy person occurs through airborne droplets (entering the mucous membrane oral cavity), as well as through everyday life (in the case of caring for a patient, through dirty hands). There is a possibility of introduction of microorganisms through infection on damaged areas of the skin. 
Treatment of streptococcal infection
If a person is diagnosed with streptococcus in a smear, timely treatment is important. Experienced doctors give preference to antibiotics of the penicillin category: the drugs “Benzylpenicillin”, “Ampicillin”. If the patient is intolerant to this type of antibacterial agent, treatment is carried out with the drug "Erythromycin". After antibiotic therapy, the drugs “Linex” and “Baktisubtil” are prescribed, which restore intestinal flora. Interruption of treatment is not recommended antibacterial agents. Toxins released by streptococci are eliminated by drinking plenty of water. 
Zepping
Another method of influencing streptococci - zapping - is preferable for infectious sore throat. IN this method The infection is affected by the resonance of magnetic waves, which effectively fights bacteria. When you complete the prescribed treatment, cocci in the smear will be detected in small quantities or completely absent.
Possible complications
At the moment there is no vaccine against streptococcal infection, as it tends to mutate. Relapses are possible. In this case, it is recommended to change the treatment method, as this may indicate resistance of the infection to those already prescribed. antibacterial drugs. But don't self-medicate. After all, untreated streptococcal infection leads to diseases such as pneumonia, erysipelas, glomerulonephritis, bronchitis, tonsillitis, as well as scarlet fever, streptoderma, rheumatism, abscess, pharyngitis and many others dangerous to human health. And streptococcus in a smear of a pregnant woman is also very dangerous for the baby. Listen to the recommendations of an experienced specialist who will advise you and prescribe treatment for you, taking into account the individual characteristics of your body, and will help prevent the onset of serious diseases.
The history of streptococcal research begins in the 19th century, when streptococcus was discovered in a smear of purulent discharge from infected patients. After this, many researchers from all over the world began to actively study the bacteria, and at the beginning of the 20th century it was proven that this particular bacterium is the cause of scarlet fever. After this, many more studies were carried out, which are still ongoing.
Diseases that can be caused by streptococcus.
This bacterium has a large number of its younger relatives, which can cause a fairly wide range of diseases. All diseases have only one thing in common - in each case, streptococcus is detected in the patient's smear.
- Bronchitis
- Angina
- Erysipelas
- Pneumonia
- Periodontitis
- Abscess
- Rheumatism
- Glomerulonephritis
- Pharyngitis
- Scarlet fever
- Streptoderma
Diagnostics and identification of bacteria
There are many ways to identify this pathogen, most of which are quite technically complex. But, to put it simply, we can describe the most basic way to identify all pathological human microorganisms.
The wound or any other discharge of the patient associated with the disease is sown on some nutrient medium, in a Petri dish. After this, a pure colony is identified, that is, the growing colonies of microorganisms are repeatedly reseeded into new selective ones and all sorts of methods of influence are applied to them, which bacteria of one type cannot tolerate, while other bacteria easily survive. After long weeks and sometimes months of work on a Petri dish, a pure culture of the pathological microorganism must be isolated, which is stained with various dyes and identified by various means.
If time does not allow you to perform this long microbiological ritual, then there are methods for express diagnosis of microbes, one of which involves microscopy of the discharge. If, as a result of a rapid examination, cocci are detected in the patient’s smear, and the symptoms coincide with the expected disease, then the microbiologist can begin more detailed treatment, and the doctor can begin treating the patient.
Treatment and prevention
Once the disease is diagnosed, treatment can begin. are not proof of presence in the body, but can serve as one of the facts, along with other tests, that can speed up the process of identifying the microbe if streptococcus is actually detected in the smear.
It is successfully carried out using antibiotic therapy. It is important not to be independent in this matter and entrust the choice of antibiotic to a doctor, otherwise there may be Negative consequences for the patient’s body in the future - from an uncured disease, due to an incorrectly selected drug, to the development of resistance of microorganisms to drugs.
Today there is no stable vaccine against development, which is associated with the high variability of this microbe, therefore, after streptococcus has been detected in a smear, treatment with antibiotics is carried out until full recovery patient. In case of relapse of the disease, in most cases it is necessary to change the treatment method, because the relapse may be associated with microbial resistance to the selected drugs.
Website - medical portal online consultations with pediatric and adult doctors of all specialties. You can ask a question on the topic "streptococcus in the vagina" and get it for free online consultation doctor
Ask your questionPopular articles on the topic: streptococcus in the vagina
Vaginal discharge - which are considered normal, and which are a symptom of the disease and require immediate treatment. In order to preserve your youth and women Health on long years Let's understand thoroughly the problem of vaginal discharge.
A new antifungal drug Zalain for the treatment of acute vulvovaginal candidiasis
The share of vulvovaginitis caused by fungal infection is 24-36% in the structure of infectious diseases of the vulva and vagina. A number of predisposing factors are of great importance in the occurrence and increase in the frequency of cases of vulvovaginal candidiasis...
Modern view on the problem of bacterial vaginosis
Bacterial vaginosis (BV) – infection vagina, characterized by a dysbiotic state of the vaginal biotope with an increase in the number of opportunistic microorganisms, a decrease and change in qualitative and quantitative...
Vaginitis and vaginosis are the most common diseases of the genital organs in women. The diseases themselves do not seem to pose a serious threat. But their complications... Find out why vaginitis and vaginosis must be treated only by a gynecologist, and not otherwise
Vaginitis - inflammation of the vaginal mucosa can be caused by various pathogens (fungi, E. coli, Trichomonas, gonococci, chlamydia, etc.). Read how dangerous the disease is and why self-medication is unacceptable in our article.
Bacterial vaginosis: some aspects of etiology, pathogenesis, clinical picture, diagnosis and treatment
Currently, one of the most common obstetric and gynecological diseases are vulvovaginal infections, of which 30-50% are bacterial vaginosis. According to the definition of many authors, bacterial vaginosis is a dysbiosis...
Mucous membranes are an important part of the body's protective barrier
Normal functioning of the human body involves maintaining conditions internal environment, which differ significantly from external environmental conditions. The area of contact between these two environments is critical to the integrity of the whole...
Trichomoniasis is one of the most common diseases of the genitourinary tract and ranks first among sexually transmitted diseases. According to the World Health Organization (1999), 10% of the world's population is affected...
Ask your questionQuestions and answers on: streptococcus in the vagina
2014-11-21 09:21:31
Laura asks:
Hello
Streptococcus was found in the vagina, 10^6
Lactobacilli 10^5
Slight pain with PA at the entrance to the vagina
There's nothing else to worry about. But upon examination, everything is red and yellowish thick discharge
Leukocytes at the upper border
Urine culture also showed staphylococcus 10^5
The gastroenterologist diagnosed mild dysbacteriosis, enterol + stimbifid
What should I do? No one wants to treat my problems comprehensively. Is it possible without antibiotics?
Answers:
Hello! Dysbacteriosis does not require antibacterial therapy at all - antibiotics do not solve, but only aggravate the problem. The gastroenterologist's tactics are correct - he is trying to restore the composition of the intestinal microflora. In the presence of vaginal dysbiosis, therapy with oral probiotics is supplemented with intravaginal therapy ( vaginal suppositories, the components of which restore the vaginal microflora). At the same time, the doctor (gastroenterologist or gynecologist) must look for the cause that led to the disturbance in the composition of the vaginal microflora and gastrointestinal tract- it can be different medications, chronic diseases organs of the gastrointestinal tract and upper respiratory tract, severe stress, etc. In addition, you should undergo an extensive examination by a urologist - you need to find out what is causing the appearance of staphylococcus in the urine and, if necessary, undergo adequate treatment of the identified pathology. Thus, three doctors - a gastroenterologist, a urologist and a gynecologist - should be involved in correcting the disorders discovered in you. Take care of your health!
2016-10-20 09:31:43
Olga asks:
Hello, this is the situation - we were worried copious discharge and a slight unpleasant odor, as well as discomfort and pain during sexual intercourse - a course of fluconazole was completed for 7 days, 0.100 units each, in parallel, Terzhinan vaginal suppositories for 10 days and douching, then metronidazole for 7 days, 3 tablets three times a day, as a result the smell disappeared and the discomfort also disappeared, but the heavy discharge is disturbing, and after a course of taking medications, they were taken quantitative analyzes for microinfections: - chlamydia, ureaplasma, mycoplasma, gardnerella - none of this was detected - 0, also gynecological smear on flora - Flat epithelium (V) - a little, Leukocytes (V) - 1-2, Key cells (V) - not detected, Fungal elements (V) - not detected, Microflora (V) - mixed, Amount of microflora (V) - moderate, Flat epithelium (C) - single, Leukocytes (C) - 10-15, Key cells (C) - not detected, Fungal elements (C) - not detected, Microflora (C) - mixed, Number of microflora (C) - scanty, squamous epithelium (U) - moderate,
Leukocytes (U) - 0-1, Key cells (U) - not detected, Fungal elements (U) - not detected, Microflora (U) - mixed, amount of microflora (U) - scanty, Neisseria gjnorrhoeae - not detected, Trichomonas vaginalis - not detected. Even after the treatment, I took a 10-day course of vaginal suppositories to restore the vaginal flora, it became better, but there was no discharge severe pain still bothers me, but no longer smells, especially during sexual intercourse (previously, the right ovary was injured during sexual intercourse, was in hospital treatment, after treatment there are adhesions). Please tell me, judging by the results of the tests, whether it is possible to paint a picture as a whole, since I am temporarily in another city and there is no opportunity to visit a qualified specialist. From the moment of treatment, sexual contact was protected and remains so to this day. After a while, the sexual partner was diagnosed with lichen planus on the mucous membrane of the penis, I know that it is not transmitted, the tests are normal (I think it is connected with the nervous and immune system), but the doctor added that streptococcus was detected, tell me it is transmitted Is streptococcus sexually transmitted and what type is it? Thank you in advance!
Answers Gerevich Yuri Iosifovich:
Good afternoon. Apparently there was bacterial vaginosis, maybe candidiasis, you need to restore the normal flora of the vagina - do a tank culture; lactobacilli should predominate there and there should be no pathological flora - have sexual intercourse with a condom until the partner is cured. Pay attention to maintaining hygiene. Streptococcus is not transmitted sexually.
2016-04-29 18:40:47
Lily asks:
Hello! Please help me understand the problem. After my partner and I stopped using condoms, the first time after sexual intercourse I developed cystitis (cured with furagin), the second time - itching and burning in the vagina. I contacted a gynecologist. A diagnosis was made: vulvovaginitis, cervicitis. The doctor took a general smear and an analysis for microflora and STDs. A general smear revealed a slight increase in the number of leukocytes (10-15), no STDs were detected, microflora analysis showed an increase in the number of streptococci. Mycoplasma, candida, and gardnerella were not detected. The number of lactobacilli is normal.
She was treated for streptococcus with fluomizin. After that, all the symptoms went away, benchmark analysis(bacterial culture and general smear) are normal.
The partner consulted a urologist and was tested for STDs (including ureaplasma, mycoplasma, candida and HPV viruses And herpes simplex), also handed over the tank. culture with antibiotic sensitivity - everything is clear.
Could it be that when pure analyzes Do I have this reaction to my partner? I've heard about microflora incompatibility. I've never had anything like this happen with any partner before.
Are there any tests to check the compatibility of microflora? What are some ways (that do not interfere with conception) to prevent symptoms of vaginitis? Should your partner be treated for streptococcus “just in case”?
I also heard that such troubles can arise when immunity decreases. Maybe it’s worth contacting an immunologist, or is it too early to sound the alarm?
Thank you in advance for your response.
Answers Serpeninova Irina Viktorovna:
2016-03-06 20:18:48
Lily asks:
Hello! I wanted to ask you for advice.
After my partner and I stopped using condoms, the first time after sexual intercourse I developed cystitis (cured with furagin), and the second time - itching and burning in the vagina. I contacted a gynecologist. A diagnosis was made: vulvovaginitis, cervicitis. The doctor took a general smear and an analysis for microflora and STDs. A general smear revealed a slight increase in the number of leukocytes (10-15), no STDs were detected, microflora analysis showed an increase in the number of streptococci. Mycoplasma, candida, and gardnerella were not detected. The number of lactobacilli is normal.
The doctor prescribed me vaginal tablets Fluomizin. After their use, the symptoms of vaginitis decreased, but some discomfort are still preserved (possibly by-effect from the drug itself).
With a partner for now sex life stopped. The fact is that in the absence of sexual activity and when using condoms, I did not have such health problems... All the troubles begin only a day after unprotected sexual intercourse.
The questions are:
1) should I send my partner to the doctor and what tests should he undergo? Do you need treatment now? young man from streptococcus?
2) What are the ways to protect yourself from relapse after PA, besides condoms?
3) Is Fluomizin alone enough? Maybe more immuno-strengthening drugs are needed (1.5 years ago I was treated for chronic vaginitis associated with ureaplasma, the treatment was successful)?
Thanks in advance for your answer.
Answers Yushchenko Tatyana Aleksandrovna:
Hello! It is advisable to consult a urologist for your sexual partner. Men often have chronic prostatitis associated with the presence of pathogenic or conditionally pathogenic microflora. You can protect yourself from relapse of vulvovaginitis after sexual intercourse by using products such as Miramistin or the same Fluomizin suppositories, which can be used immediately after sexual intercourse. Fluomizin alone is enough, but I would do such an analysis as a tank. vaginal culture with sensitivity to antibiotics. Then it would be possible to select a more specific drug for treatment.
2016-03-06 17:48:23
Irina asks:
Good afternoon. I haven’t been able to recover for a year now. After taking Levofloxacin, a burning sensation began in the vagina, which turned into inflammation. A smear on the flora showed the presence of streptococcus anhaemolyticus 10 to 5 degrees. She was treated with oral antibiotics and Terzhinan suppositories, after a suppository with lactobacilli. But
Nothing helped. The doctor prescribed me to drink Bifiform - to restore the flora from the inside. I drank for 3 months and also tried all sorts of antifungal suppositories and suppositories with lactobacilli. I came to the conclusion that suppositories with lactobacilli make me feel better and everything seems to go away, but as soon as I quit it all comes back and terrible inflammation begins. I have been using all kinds of suppositories with lactobacilli for almost a year now. I took a stool test for dysbacteriosis, was cultured for klebsiella pneumoniae grade 10 to 7, was treated with antibiotics, I have been using suppositories with bacteria as I have, but as soon as I quit, everything comes back again. What should I do, this is an endless routine. I ask you to help me.
Answers Medical consultant of the website portal:
Hello Irina! It is necessary to re-culture vaginal discharge and be tested for sexually transmitted diseases. Perhaps you should change your gynecologist. It is possible that examination for diabetes, condition assessment immune system and re-evaluation of the gastrointestinal tract. Take care of your health!
2015-10-15 14:35:30
Anonymous asks:
Please tell me. I was preparing for metrosalpingography. I took a vaginal smear. Enterococcus fecal was detected. I was treated with Neotrizol suppositories, Ofloxacin for 5 days and Itrungar for 5 days, and had a control smear. Hemolytic streptococcus was found in this smear. I was treated with Flemoklav for 7 days and Betadine suppositories. I took a control smear again and it showed Escherichia coli, and all this over a period of 1.5 months. I do not know what to do. And why does it show something new every time?
Answers Bosyak Yulia Vasilievna:
Hello! Enterococcus and Escherichia coli can appear in the vagina exclusively from anus, therefore, there may be several reasons for identifying infections - incorrect personal hygiene (wearing thongs, for example), problems with the rectum (hemorrhoids), anal sex. Think about what could be the reason and rule it out.
2015-06-05 17:38:40
Sofia asks:
Bacterioscopic examination of discharge from the MPS
Type of study Result
Bacterioscopic examination of discharge from the MPS in women
CERV. Red blood cells in small quantities
Epithelium CERV Flat in a small amount, cylindrical in a small amount
Leukocytes CERV 20-25 in the field of view
CERV mucus in significant quantities
Flora: CERV Mostly rod moderate
Dederlein sticks CERV In moderation
Comma Variabile CERV In small quantities
Suppurative: CERV
- staphylococci CERV Not detected
- streptococci CERV Not detected
Various cocci CERV Gr(+), Gr(-) in small quantities
Trich. vaginalis CERV Not detected
Gonococci CERV Not detected
VAGIN. Red blood cells in small quantities
VAGIN Squamous epithelium in small quantities
Leukocytes VAGIN 12-15 in the field of view
VAGIN mucus In moderation
Flora: VAGIN Mostly abundant rods
Dederlein sticks VAGIN in large quantities
Comma Variabile VAGIN In small quantities
Pyogenic: VAGIN
- staphylococci VAGIN Not detected
- VAGIN streptococci Not detected
Various cocci VAGIN Gr(+), Gr(-) in small quantities
Trich. vaginalis VAGIN Not detected
Gonococci VAGIN Not detected
U.R.
Epithelium UR Flat in a small amount, cylindrical in a small amount
Leukocytes UR 1-2 in the field of view
Mucus UR In small quantities
Flora: UR Mostly rod moderate
Dederlein sticks UR In moderation
Comma Variabile UR In small quantities
Pyogenic: UR
- staphylococci UR Not detected
- streptococci UR Not detected
Various cocci UR Gr(+), Gr(-) in small quantities
Trich. vaginalis UR Not detected
Gonococci UR Not detected
CONCLUSION III degree vaginal cleanliness. Elements of the yeast-like fungus type were discovered.
Is it badly neglected? Any recommendations?
Thank you in advance!
2015-04-17 08:44:16
Ekaterina asks:
Hello.
Such situation.
We have not been able to get pregnant for more than a year; we have a history of miscarriages followed by curettage (the cause was determined to be genetic).
According to ultrasound for several years, either endometrial hyperplasia or not. At the moment, after the drug cyclodinone, it is not there. There is also thrush in the throat, I suspect in the vagina too, but the analysis does not show this. At the same time, nystatin makes it better.
They checked for STDs. For 4 years now, doctors have been constantly treating something, chlamydia was found in the state hospital, but in the independent Invitro there is no chlamydia. Then gardnerella, staphylococcus, enterococcus, Escherichia coli were all treated with antibiotics and so on in a circle endlessly. The microflora has already been killed, there is no immunity, urethritis constantly bothers me, sometimes with cystitis. According to the latest data, the smear is without inflammation and at the same time urethritis-cystitis is tormenting, the culture shows Streptococcus agalactia 10v5. I also noticed at the same time that there is a problem with my throat, it hurts. Many doctors were bypassed. One said to cover all STDs with provocation, which we haven’t done yet. Name TRICHOMONADENE FLUOR INEL, tell me how harmless this is and does this make sense, will the analysis really be MORE ACCURATE?????

