Genital warts in women. Why condylomas occur, methods for removing formations and principles of HPV treatment.
The human papillomavirus in women has many manifestations. Warts, dysplasia and cervical cancer are the main manifestations of the infection. Treatment of manifestations of a viral infection is not always successful. Prevention of the disease is based on the timely detection of diseases, safe sex and strengthening the immune system.
Viruses are extremely widespread among people all over the planet. They infect up to 70% of the world's population.
Do genital warts disappear?
This occurs mainly in cases where the warts are small in size and number. Warts that do not go away on their own can be treated, although it is possible to recur and reapply. The recurrence rate depends on the treatment regimen and individual circumstances. It is estimated that on average 30% of genital warts recur and almost three treatments are required.
There are two main methods of treatment: gels and creams, which are applied by the patient himself, or treatment, which is carried out by a doctor. There is no data to indicate which method is more effective. Medical treatment may include. All treatments can cause irritation and discomfort in the treatment area, as well as changes in skin color.
- Non-oncogenic types of HPV are the cause plantar warts, youthful flat and vulgar warts.
- Oncogenic types of papillomaviruses of a low degree of malignancy are the cause of the development of genital warts, endourethral and genital warts of the anus.
- 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59 and 68 oncogenic types of papillomaviruses high degree malignancies cause cancer of the vulva and anal area, vagina and cervix
Today, more than 40 types are known associated with the development of diseases of the genital organs and the perianal region.
Should you avoid intercourse when you have genital warts?
Genital warts affect pregnancy and childbirth
During pregnancy, genital warts can increase in number due to changes in the body's immune system. Therefore, their treatment may be delayed after birth to see if they disappear on their own.Very rarely, bearded formations can appear in the throat of a newborn. Caesarean section is not recommended as a precaution against this phenomenon. Genital warts, also called venereal warts and genital warts, are one of the most common types of sexually transmitted infections.
How is the human papillomavirus transmitted?
- Sexual transmission of the infection is the main one. Frequent change of sexual partners, oral-genital and anal sex greatly increase the risk of the disease. Most often, HPV infection is recorded at the age of maximum sexual activity (18-35 years). The frequency of registration of dysplasia and cervical cancer increases significantly after 30 years. The maximum number of sick women falls on the age of 45 years.
- Infection of a newborn can occur during childbirth from an infected mother. The disease in them manifests itself at the age of 5 years and is characterized by the appearance of multiple papillomas in the larynx (respiratory papillomatosis).
Important in relation to the timely diagnosis of HPV infection is the fact of a long (months and years) incubation period and often asymptomatic course of the disease.
Genital warts soft growths that occur on the genitals. Genital warts, a sexually transmitted infection caused by certain strains of the human papillomavirus. These skin lesions can cause pain, discomfort, and itching.
What are genital warts?
This article will look at the causes, diagnosis and treatment of genital warts. We will also discuss possible complications and how to avoid them. Facts about genital warts. Here are some key questions about genital warts. Genital warts are contagious they are caused by the papilloma virus that affects the skin The biggest risk factor for genital warts is sex before prophylaxis Some genital warts respond well to topical medications. Genital warts infected are manifested by a fleshy growth on the vulva or anus, consisting of fibrous formations covered with compressed epithelium.
Rice. 1. In the photo, the human papillomavirus.
How the disease develops
The human papillomavirus in women first penetrates into the epithelial (superficial) layer of the skin or mucous membranes. The penetration of viruses occurs through injured areas that occur as a result of microtrauma, abrasions or inflammation.
Genital warts are caused by sexual contact with a person infected with the human papillomavirus; They are usually benign, but many subtypes have the potential for malignant changes. Genital warts based on the male penis.
It is estimated that 65% of people with sexual relations with a person who has genital warts will infect and develop them. Genital warts often appear about three months after infection - but in some cases there may be no symptoms for many years.
Epithelial cells begin to divide intensively, which is manifested by the appearance of specific growths on the surface of the skin or mucous membranes in the form of warts. Due to the inability of epithelial cells to support the reproduction of viruses, the production of viral particles on this stage not happening.
The site of virus replication is highly specialized epithelial cells located on the basal layer. As a result of the reproduction of viruses, the inner layer of the epidermis is deformed and thickened.
Other risk factors for genital warts
About 14 million people become infected each year. Who are the most important factors that cause genital warts? Ask yourself the following questions, as your doctor is likely to ask the same questions when you go for testing. Genital warts are common among teenagers, teenagers and young adults. Do you have a severe infection or take medications that damage the immune system? blood cancers like leukemia change our immune cells and make them dysfunctional. Drugs such as steroids reduce our immune system over time. Have you noticed any damage to the skin of the genitals? They give the virus a chance to enter your body. Sex unprotected sex with different partners having sex with someone whose sexual history you don't know Oral sex increases the risk of developing genital warts in the mouth or throat early age stress and others viral infections, in the same time.
Complications of genital warts
In addition, the hormonal changes that occur during pregnancy can cause genital warts to appear, bleed, or increase their number.
- How many sexual partners do you have?
- The more partners, the more likely it is to get the virus.
- Do you use condoms?
Virus-infected basal layer cells are a constant source of viruses for new epithelial cells. Since the active assembly of new viral particles and their release from cells occurs in the keratinized layer of the epithelium, it is these areas that are especially dangerous in relation to infection that occurs by contact.
People should go consider if. A doctor can usually diagnose genital warts, if any. The examination may include examination of the vagina or anus. In rare cases, a wart biopsy may be needed. Sometimes, even if you find a wart, the doctor or nurse may ask the patient to come back later. Visible warts may not appear immediately after infection.
See how genital warts?
Various forms of genital warts that affect women can occur in or around the vagina, vulva, anus or at the entrance to the uterus. Often warts are too small to see or notice. Warts in the vagina or anus may cause discomfort but do not cause any symptoms.
The basement membrane connects the epithelium layer with the layer connective tissue providing support for them. Destruction of the basement membrane leads to the development of a cancerous tumor. When viruses spread to a layer of connective tissue located under the basement membrane, a sarcoma develops.
The human body in 90% of cases is able to get rid of viruses on its own. But if the immune system is not able to stop the growth of viral particles, a malignant disease develops.
In men, genital warts are not as common as in women. They often appear on the top of the penis, but can occur around the anus, especially when the virus is transmitted during anal sex. Most types of warts appear one to three months after infection. If you think you are infected, you should study in order to avoid complications and prevent transmission of the infection to future partners. About half of all cases of genital warts occur on the shaft of the penis, usually just below foreskin.

Rice. 2. Scheme of development HPV virus- infections.
Genital warts (warts)
Genital warts in women
Human papillomaviruses in women of types 6 and 11 are in 90% of cases the cause of the development of genital warts. The growth of genital warts is caused by human papillomaviruses, which have low oncogenic activity. Genital warts grow outward (exophytic growth). Them appearance recalls cauliflower or cockscomb. They are soft in texture. They have a pinkish color.
In one out of every three cases of genital warts around the anus in one out of ten cases of genital warts on the glans penis in one out of ten cases of genital warts in urethra in one of twelve cases of genital warts under the foreskin in about thirty cases of genital warts appear between the anus and scrotum. In one hundred cases, genital warts of the scrotum. Doctors will only treat patients who have visible warts.

Treatment is aimed at eliminating visible warts and reducing the number of existing viruses. If the amount of virus can be reduced, the patient's immune system is more likely to fight them. These treatments are effective in removing warts.
Genital warts in women are located in the region of the labia minora, the entrance to the vagina, the cervix, anus and anal canal, less often - in inguinal region and perineal areas. Pain during bowel movements, severe itching and spotting are symptoms of genital warts located in the rectum. Increased secretion of leucorrhoea, the appearance of sanious discharge or blood after intercourse are the main symptoms of genital warts located on the mucous membrane of the cervix or vagina.
Topical medications - A cream or liquid is applied directly to the wart for a few days each week. This can be used at home or in the clinic - depending on the type of treatment. As the skin heals, the lesions slide off, allowing the appearance of new skin. Sometimes multiple treatments are required. The patient is usually placed local anesthetic. Surgery - the wart is removed. Will use local anesthesia.
- Treatment may continue for several weeks.
- Freezing causes blisters to form around the wart.
Condylomas can appear on the mucous membrane of the tongue, the inner surface of the cheeks, the red border of the lips and the palate.
Genital warts sometimes show a tendency to merge. In some patients, warts merge to form one giant condyloma (Buschke-Levenshtein warts). Such warts are prone to maceration and decay.
The treatment is not painful, but can sometimes be uncomfortable with some soreness and irritation for one or two days. Pain can be taken from patients after treatment. Some patients feeling pain may find that a warm bath helps. After the bath should be completely dry place. Patients should not use bath oils, soaps, and creams until treatment is complete.
Genital warts usually disappear eventually, even if left untreated. Sometimes they become large in size and take up large spaces without treatment. Experts say that untreated genital warts are not harmful to the health of an infected person, but may be uncomfortable to look attractive. However, treating warts greatly reduces the risk of transmission to another person.
The location of genital warts in the cervical canal or on the cervix is an unfavorable factor due to the possibility of developing cancer.
What causes oncogenic transformation of genital warts
- Early onset of sexual activity, frequent change of sexual partners, neglect of condom use, multiple pregnancies, injuries cervical canal and anogenital contacts.
- The combination of human papillomavirus with gonorrhea, trichomoniasis, chlamydia.
- The risk of developing oncogenic transformation increases significantly when HPV is combined with gonorrhea, trichomoniasis, and chlamydia.
- Long term use of oral contraceptives.
- Hypovitaminosis A and C, folic acid and b-carotene.
- Smoking and alcohol abuse.
- Unsatisfactory living conditions.
In 90% of cases, genital warts undergo regression. At 10% are transformed into cancerous tumor.
Usage improper treatment can do more harm than good. Some home remedies are advertised as being helpful in treating genital warts, but there is little evidence to support them. Always check with your doctor before trying home treatments.
How to prevent genital warts?
The sexual disease was also called genital warts or figs.
Condylomata, Czech genital warts or venereal warts, acute warts, figs - an infectious viral disease. The risk of transmission is significant in vaginal and anal sex, with oral sex the risk of infection is reduced.

Rice. 3. In the photo, genital warts.

Rice. 4. In the photo, genital warts in women.

They occur during sputum abnormalities, in moist patches on the genitals, in the groin, or around the rectum. The living soil of this disease is low level personal hygiene. The disease often has a faster and stronger gradient if it occurs with vaginal inflammation or during pregnancy.
Genital warts are more common with phimosis, inflammation urinary tract and vaginas. The presence of warts in the rectum increases the risk of anal intercourse. Some sources report an increase in risk of up to 800%. Genital warts are very common and continue to grow. It is one of the most common sexually transmitted diseases in the Czech Republic. Among the most affected groups are young women in their twenties and gay men.
Rice. 5. In the photo, genital warts.

Rice. 6. In the photo, genital warts in the inguinal region.

Rice. 7. In the photo, genital warts on the tongue.
Flat warts in women
The growth of flat condylomas in women is caused by human papillomaviruses, which have a high oncogenic activity. Flat warts grow deep into the epithelium. Most often, flat warts are located in the cervix and vagina. Reveal this species condyloma is possible only with the use of special types of research.
The presence of genital warts of any kind is an indication for a biopsy and histological examination of the biopsy material.
![]()
Rice. 8. The photo shows a flat condyloma.
Giant condyloma of Buschke-Levenshtein
Giant condyloma Buschke-Levenshtein is a very large genital warts. Its development is associated with human papillomavirus types 6 and 11.
Large and small labia - frequent places localization of giant condyloma in women. Condylomas can be located in the perianal and anorectal regions, less often in the groin and oral cavity. Failure to work leads to malignancy of condyloma immune system.
The disease begins with the appearance of several genital warts, which eventually merge with each other. Vegetations form on the surface of the formation, which eventually become covered with scales. Maceration of surface elements leads to the appearance bad smell. The massiveness of papillomatous growths and invasive destructive growth are the main symptoms of the disease.
The giant condyloma of Bushke-Levenshtein grows slowly, gradually growing into soft tissues. Over time, squamous cell carcinoma develops. Excision of genital warts followed by cryodestruction is the main method of treatment.

Rice. 9. In the photo of Bushke-Levenshtein condylomas.
Diagnosis of genital warts
Condylomas in women are easy to identify visually. However, in some cases, a test using 3% acetic acid is used. The essence of the test is that a medical napkin soaked in a solution of acetic acid is applied to the surface of the formations for 10 minutes. At the same time, condylomas acquire a whitish color. If a precancerous disease or cancer is suspected, a biopsy is performed.

Rice. 10. In the photo positive test with 3% acetic acid for cervical lesions (left) and genital warts (right). The test allows the doctor to determine the boundaries of the damage.
When removing genital warts, the risk of developing an oncological process does not decrease. An annual examination by a gynecologist and a cytological examination of smears from the cervix is the main method for early detection of cervical cancer.
Treatment of genital warts
Existing methods of treating genital warts do not always lead to the expected result.
Condylomas in women often recur, as they are able to remain inactive for a long time in the thickness of the epithelium, which makes them invisible during examination.
When using condoms, the risk of transmission of infection to a sexual partner is reduced, but does not completely disappear.
Treatment of warts with physical methods (removal of warts)
- Electrocoagulation is a widely used method for removing genital warts. Its efficiency reaches 85 - 95%. Long-term non-healing defects and scars with subsequent stenosis are complications of electrocoagulation.
- Laser surgery also provides good effect. for a long time non-healing wounds, the addition of a secondary infection, scarring and recurrence are complications of using this technique.
- At the core radio wave surgery lies the evaporation of the liquid part cellular composition under the influence of high frequency radio waves (device "Surgitron" and "Ellman").
![]()
Rice. 11. When removing warts with the help of radio wave surgery, the Surgitron apparatus is used. On the right - electrodes to the device.
Electrocoagulation, removal of genital warts with a laser and radio waves requires preliminary anesthesia.
- Cryodestruction (freezing) is a commonly used method. At the core this method treatment of the affected surface with liquid nitrogen lies. Low cost and rare development of scar tissue are the advantages of cryodestruction.
Removal of genital warts with the use of medications
Removal of genital warts using the application medications based on the action of highly concentrated solutions chemical substances on damaged tissue.
- Trichloroacetic acid 80 - 90% concentration when applied to the area of damage causes coagulation necrosis.
- Salicylic-resorcinol collodion (varnish). Salicylic acid and resorcinol, which are part of the drug, have a pronounced destructive effect. Inflammation, pain syndrome and prolonged healing are the disadvantages of this technique.
- A drug Solcoderm contains organic and inorganic acids. Solcoderm is used for warts, located on open areas of the skin and mucous membranes of the genital area and anus. When the drug is applied, the patient experiences severe pain and burning.
- Podophyllin obtained from plants P. peltatum and P. emodi in the form of resin.
Use the drug in the form of a 30% alcohol solution.
- podophyllotoxin derived from podophyllin. An alcohol solution of this drug is used only for condylomas located on the external genitalia.
- Condylin (podophyllotoxin) can be used on its own. The method of application is described in detail in the instructions.
- 5-fluorouracil (cream) is a cytostatic. Under its influence, the synthesis of viral DNA is disrupted. The drug is used in the treatment of warts, located intravaginally in women and endourethral in men.

Rice. 12. In the photo, Solcoderm is a remedy for removing genital warts.

Rice. 13. In the photo, Podophyllin and Podophyllotoxin are means for removing genital warts.
Antivirals
- Interferons (IFN) are cytokines that are produced by human cells in response to the introduction of viruses. Information about the effectiveness of drugs is contradictory. In some cases, they significantly improve clinical dynamics and improve the quality of therapy.
- Panavir is an antiviral drug plant origin. The drug is available in the form of a solution for intravenous administration, gel for external use and rectal and vaginal suppositories.

Rice. 14. In the photo antiviral drug Panavir.
cervical dysplasia
Cervical dysplasia develops at the border where the epithelium of the cervical canal (cylindrical or glandular) passes into the epithelium of the vaginal part of the cervix (stratified squamous).
Changes that occur in the mucous layer of the cervix, but do not affect the basement membrane, are called cervical dysplasia. Epithelial cells changed under the influence of viral particles are called atypical. In such cells, the process of maturation and differentiation is disrupted. The number of atypical cells detected during histological examination, depends on the degree of violation of cell differentiation and the area of the affected epithelium. Sometimes several areas of dysplasia are recorded.
Till pathological process localized within the epithelial layer and does not affect the basement membrane, a cancerous tumor does not develop.
With the destruction of the basement membrane, the pathological process spreads to neighboring tissues and regional The lymph nodes. Squamous cell carcinoma develops from epithelial cells. Sarcoma develops from connective tissue cells.

Rice. 15. In the photo, cervical dysplasia.
Human papillomavirus and - the main etiological factors development of uterine dysplasia. They are transmitted sexually. early and disorderly sex life, neglect in the use of contraceptives, frequent change of sexual partners contribute to the development of the disease. The risk of degeneration of dysplasia into a cancerous tumor ranges from 40 to 64%.
It is believed that human papillomaviruses with low oncogenic potential - types 6, 11, 40, 42, 43, 44 cause dysplasia mild degree, and viruses of high oncogenic risk - 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68, 73, 82 and possibly 26, 53 and 6 types, cause cervical dysplasia uterus of moderate and severe degree.
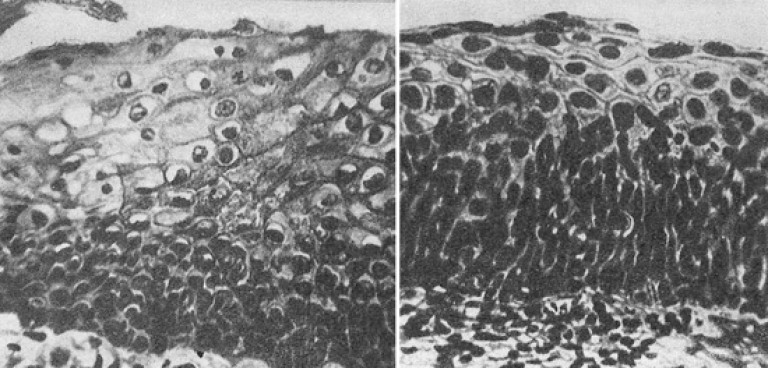
Rice. 16. In the photo different degrees cervical dysplasia.
A mild degree of cervical dysplasia (photo on the left) is characterized by the proliferation of epithelial cells only in the area where the basement membrane is located. With a severe degree of dysplasia (photo on the right), atypical cells appear in the uppermost layers of the epithelium.
Diagnosis of dysplasia of the uterus
- At laboratory diagnostics genital warts in women are primarily used cytological method, which allows in the smears of the preparation to reveal the state of the cells of the multilayer squamous epithelium cervix.
- Colposcopy simple or extended - an integral part of the gynecological examination. Colposcopy is performed if pathological changes on the mucous membrane of the cervix. When indicated for colposcopy, a targeted biopsy is performed.

Rice. 17. Colposcopy is an integral part of a gynecological examination.

Rice. 18. In the photo, a colposcope (left) and a video coloposcope (right).
- The technique for determining the DNA of highly malignant viruses of 12 types is widely used ( polymerase chain reaction - PCR) in scrapings of the cervical canal, urethra or in the urine.
- Of the serological methods used antibody detection technique, which are formed in the patient's body on specific proteins of viruses. This test is a marker of a viral infection.
- Due to the fact that HPV infection stimulates oncogenesis, in some cases immunity indicators- the level of CD4 and CD8-lymphocytes, the level of endogenous interferons. The level of estrogens in the blood and oncogenicity proteins of the human papillomavirus E7 is determined.

Rice. 19. The photo shows severe cervical dysplasia.
Treatment of cervical dysplasia
For mild dysplasia conservative treatment. For moderate and severe dysplasia, amputation or excision with a scalpel of the affected tissues of the cervix (cone-shaped excision) and physical impact on the affected areas are used. All removed tissues are subject to histological examination.
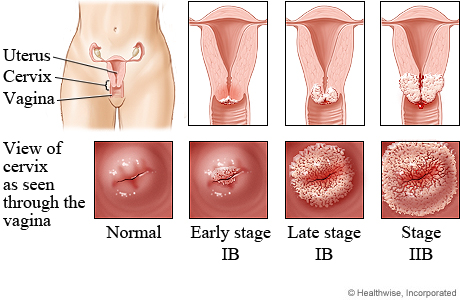
Cervical cancer
Of the 100 types of human papillomavirus, 13 are highly malignant viruses. They lead to the development of cancer of the genital organs in men and women. The most serious disease of them is cervical cancer. Its cause in 90% of cases are human papillomavirus types 16 and 18. Every year, the disease is registered in 500 thousand women, half of whom die.
Cervical cancer develops at the border where the epithelium of the cervical canal (single-layer cylindrical or glandular) passes into the epithelium of the vaginal part of the cervix (stratified squamous). Squamous cell carcinoma develops from stratified squamous epithelium (80-90% of all cases). Adenocarcinoma develops from the glandular epithelium (10-20% of cases).
How the disease develops
A virus that has penetrated the epithelium of the cervix can long years show nothing. The disease begins with cervical dysplasia. Detect dysplasia early stages its development allows oncocytology.
Cancer may not grow into the basement membrane. Such cancer is called non-invasive. Invasive cancer invades the basement membrane and spreads to fatty tissue and lymph nodes, squeezing and destroying neighboring organs. With blood flow cancer cells spread (metastasize) throughout the body.

Rice. 20. The photo shows cervical cancer.
Symptoms of cervical cancer
Bloody discharge not associated with menstruation - the main early symptom diseases. Pain in the lower abdomen, frequent and painful urination, difficulty in defecation are the main symptoms of cervical cancer on late stages. Fistula formation from the vagina into the rectum and bladder, the appearance of metastases are signs of an advanced form of cervical cancer.

Rice. 21. In the photo, cervical cancer. Bloody discharge- the main early symptom of the disease.
Diagnosis of cervical cancer
Diagnostics not invasive cancer cervix includes:
- targeted biopsy,
- cystoscopy and sigmoidoscopy.
Diagnosis of invasive cervical cancer includes:
- examination of the cervix in the mirrors,
- study of the state of internal organs,
- application modern methods research (ultrasound, computed tomography, magnetic resonance imaging, positron emission tomography and lymphography),
- biopsy.
Treatment of cervical cancer
Treatment of cervical cancer is carried out taking into account the stage of the disease. With a small tumor and a small depth of invasion, a cone-shaped excision of the affected area of the cervix or extirpation (removal) of the uterus is performed along with the tubes and ovaries and, according to indications, pelvic, and sometimes with para-aortic lymph nodes. With metastases to the lymph nodes surgical treatment supplemented with radiation or radiation + chemotherapy. Complex radical operation trachleectomy allows you to save the reproductive function of a sick woman.

Rice. 22. The photo shows the stages of healing of the wound surface after conization (cone-shaped excision of the affected area of the cervix).
Cervical cancer and pregnancy
In pregnant women, swabs from the cervix and cervical canal must be examined. If there is a suspicion of the presence of altered tissues, a biopsy is performed.
Cervical Cancer Vaccine
AT Russian Federation Two vaccines against cervical cancer are registered:
- Bivalent vaccine Cervarix protecting against 16 and 18 types of viruses.
- The quadrivalent Gardasil vaccine protects against types 16, 18, 6 and 11 of the virus.
A vaccination is considered complete if the vaccine has been administered three times. Vaccination is considered most effective at the age of 10-14 years. Vaccination of women up to 26 years of age is allowed, which is paid in our country.
Vaccination prevents about 70% of cervical cancer cases. Therefore, all women, vaccinated and not vaccinated, should be examined annually by a gynecologist with a mandatory cytological examination of cervical smears.
Safe sex, vaccination, active detection of the disease using a cytological method and timely treatment of cervical dysplasia are the most effective prevention cervical cancer.
Human papillomavirus in women is one of the most common viral diseases sexual sphere. Cervical dysplasia and cervical cancer are formidable manifestations of the disease. It is impossible to completely eliminate the human papillomavirus in women. Timely detection of the disease and strengthening of the immune system is the basis for the prevention of the disease.
Articles of the section "Papillomavirus infection" Most popularCondylomas - inflammatory processes that are of viral origin. Gynecologists attribute such neoplasms to factors that can provoke cervical cancer. Why does condylomatosis appear (genital warts in women), treatment with traditional and folk methods. Should warts be removed?
Why are formed
Genital warts appear in women on the labia and in the anus, on other parts of the body they appear less frequently. It provokes the appearance of neoplasms - the human papillomavirus, which can long time go unnoticed. So incubation period can last from several months to several years.
Ways of infection:
- unprotected intercourse - you can get infected with any type of sex;
- use of common household items with infected person- discharge from genital warts penetrates through microcracks and wounds on the skin;
- children can become infected during natural delivery if the neoplasms are located on the walls of the vagina.
Important! Condylomatosis requires immediate complex treatment, especially if neoplasms appeared on the cervix.
The virus is activated against the background of a weakened immune system, the cause of this may be stress, unbalanced diets. Often warts on intimate places appear after childbirth, because a woman is constantly subject to emotional and physical overstrain. Can cause disease uncontrolled reception medicines that disrupt the balance of microflora, the state of the immune system, the abuse of alcoholic beverages.
Condylomatosis is manifested by signs of a local nature. Genital warts can be seen with the naked eye, felt while performing hygiene procedures. If warts have arisen around the anus, a woman is worried about itching and burning in this area, there is a feeling of presence foreign object which causes great discomfort.
- burning;
- pain during sexual intercourse;
- isolation of a serous character;
- the presence of a fetid constant odor.

From the fused condylomas, a liquid begins to stand out, which smells unpleasant. A woman is uncomfortable with the constant feeling of moisture. When such neoplasms are injured by clothing or during sexual contact, foci of inflammation and severe irritation occur.
To clarify the diagnosis, it is necessary to make a PCR diagnosis in order to understand the type of virus, its amount, and the degree of damage to the body.
It is advisable to use drugs for warts small size. You can use the drugs yourself, but at the same time visit the gynecologist regularly.
Means based on imiquimod - Aldar cream, Keravort, external preparations, are dispensed by prescription. Approved for use in adolescents over 12 years of age. The duration of therapy is at least 3 months. Adverse reactions– puffiness, erosion, formation of scabs. Use the cream three times a week, wash off soapy water after 10 hours.
Condiline Nycomed - it must be used 2 times a day after 12 hours, applied only with a special applicator that is attached to the drug. The treatment regimen is to apply the drug for 3 days, then take a break for 4 days, continue treatment until the warts disappear completely. The drug is highly toxic, so it can only be used in small areas.
At home, you can treat the genitals with an antiviral spray Epigen intima - this will help stop the reproduction of the virus on early stages, does not allow it to penetrate deep into the cells. Miramistin should be used after sexual contact with an infected person. You can treat the genitals with condylomas with Oksalin ointment.

A solution of Solcoderm based on acetic, lactic, nitric and oxalic acid will help to completely remove warts at home. The drug mummifies tissues in which infected cells are present - the neoplasm falls off after a few days.
Viferon, Genoferon are immunomodulators that will help to significantly speed up the healing process.
Important! Before using any medicinal product you need to consult a doctor.
Should it be removed?
Genital warts cause a lot of inconvenience, often clinging to clothes, injured during intercourse. Neoplasms contain many pathogenic microorganisms, which can cause the development serious pathologies. Therefore, doctors recommend removing warts as early as possible.
Important! Condylomas often degenerate into malignant tumors.
Effective removal methods:
- impact on neoplasm surgical laser, which leads to the destruction of cells;
- radiosurgery removal of neoplasms using a narrow beam of high-frequency waves, the least traumatic type of operation;
- thermocoagulation - cauterization of genital warts;
- chemodestruction - burning warts with nitric acid;
- cryodestruction - freezing of neoplasms with liquid nitrogen.

Interonotherapy - substances are used to remove. Which are based on interferons, which enhances the immune system, the virus is removed naturally.
Condylomatosis during pregnancy
During pregnancy, the papilloma virus is often activated - a woman develops characteristic neoplasms. If warts arose earlier, then during pregnancy their number and size increase. The main reason is hormonal changes and weakening of the immune system.
Before starting treatment, it is necessary to weigh all the pros and cons, since there is a threat to mother and baby. Therefore, the tactics and treatment regimen for each pregnant woman is considered by the doctor on an individual basis.
The child can become infected during childbirth, cesarean section with condylomatosis do not always. If the disease is not accompanied by complications, and the neoplasms are not located in the vagina, then the woman can give birth on her own.
Treatment at home
Many women who have condylomas in intimate places are embarrassed to go to the doctor, try to eliminate the problem with folk remedies. Methods alternative medicine allow you to burn neoplasms, stop the spread of the virus. But you should always remember that self-treatment can result in unpleasant complications.
Celandine
Celandine is the leader among folk remedies to remove various types of papillomas. For treatment, use the fresh juice of the plant, or pharmacy drug. It must be applied carefully, exclusively on condyloma - if the juice gets on healthy tissues, a severe burn will occur. You can use celandine once a day.

Important! It is strictly forbidden to use celandine during pregnancy.
Iodine
Iodine is another popular remedy for cauterizing genital warts. It should be carefully applied to neoplasms with cotton swab 2-3 times a day. After a few days, the neoplasm will dry out and fall off.
When using iodine, be aware of the side reactions:
- iodine actively penetrates into cells, absorbs it thyroid, which can cause its hyperfunction;
- severe burns may occur;
- scars appear at the site of cauterization.
Important! Iodine cannot be used to remove warts on mucous membranes.
Condylomatosis - serious illness, which gives a woman a lot discomfort. It can cause miscarriage, the development of pathologies in the fetus. A woman needs to regularly visit a gynecologist, when planning a pregnancy, undergo a comprehensive examination, and do an analysis for the presence of the human papillomavirus.